Cobra Election Form
Cobra Election Form - Plans cannot require qualified beneficiaries to pay a premium when they make the cobra election. After the plan receives notice of a qualifying event, it must provide the qualified beneficiaries with an election notice within 14 days. Cobra requires continuation coverage to be offered to covered employees, their spouses, former spouses, and dependent children when group health coverage would otherwise be lost. After receiving a notice of a qualifying event, the plan must provide the qualified beneficiaries with an election notice within 14 days. Plans must provide at least 45 days after the election (that is, the date the qualified. Explore cobra continuation coverage options, eligibility, and benefits for workers, families, and advisers under hipaa regulations.
Plans cannot require qualified beneficiaries to pay a premium when they make the cobra election. After receiving a notice of a qualifying event, the plan must provide the qualified beneficiaries with an election notice within 14 days. Plans must provide at least 45 days after the election (that is, the date the qualified. After the plan receives notice of a qualifying event, it must provide the qualified beneficiaries with an election notice within 14 days. Explore cobra continuation coverage options, eligibility, and benefits for workers, families, and advisers under hipaa regulations. Cobra requires continuation coverage to be offered to covered employees, their spouses, former spouses, and dependent children when group health coverage would otherwise be lost.
After receiving a notice of a qualifying event, the plan must provide the qualified beneficiaries with an election notice within 14 days. Explore cobra continuation coverage options, eligibility, and benefits for workers, families, and advisers under hipaa regulations. Plans cannot require qualified beneficiaries to pay a premium when they make the cobra election. Cobra requires continuation coverage to be offered to covered employees, their spouses, former spouses, and dependent children when group health coverage would otherwise be lost. Plans must provide at least 45 days after the election (that is, the date the qualified. After the plan receives notice of a qualifying event, it must provide the qualified beneficiaries with an election notice within 14 days.
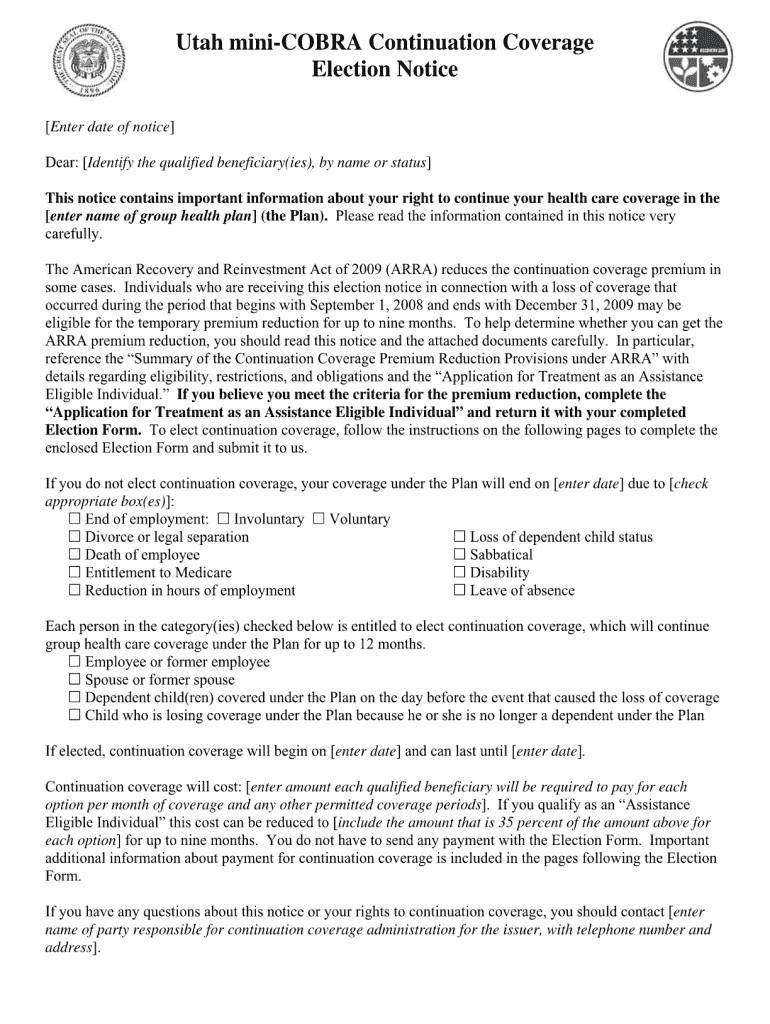
Cobra Letter Template Template and guide airSlate SignNow
After the plan receives notice of a qualifying event, it must provide the qualified beneficiaries with an election notice within 14 days. After receiving a notice of a qualifying event, the plan must provide the qualified beneficiaries with an election notice within 14 days. Plans cannot require qualified beneficiaries to pay a premium when they make the cobra election. Plans.
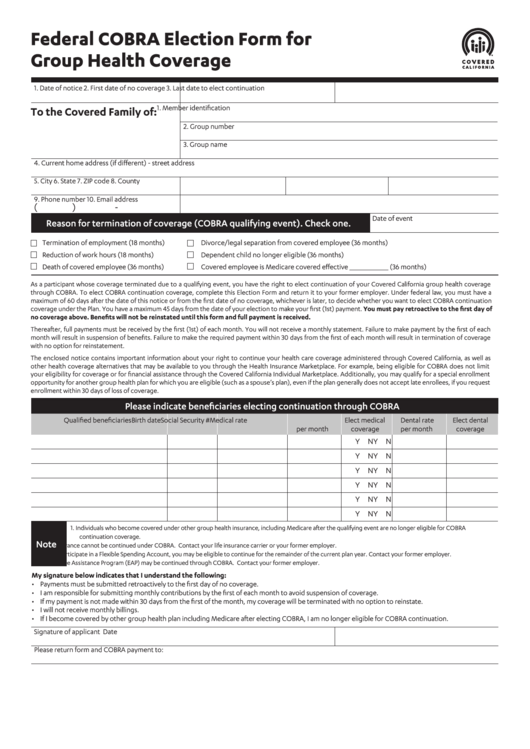
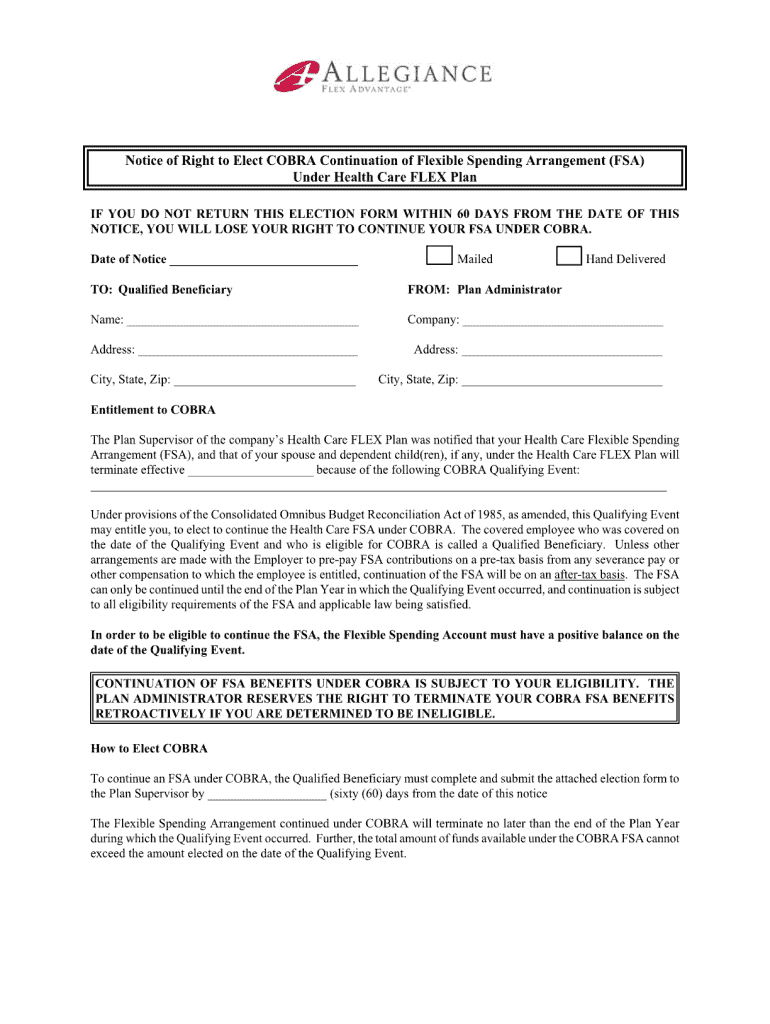
Federal Cobra Election Form For Group Health Coverage printable pdf
Plans cannot require qualified beneficiaries to pay a premium when they make the cobra election. After the plan receives notice of a qualifying event, it must provide the qualified beneficiaries with an election notice within 14 days. Plans must provide at least 45 days after the election (that is, the date the qualified. Explore cobra continuation coverage options, eligibility, and.
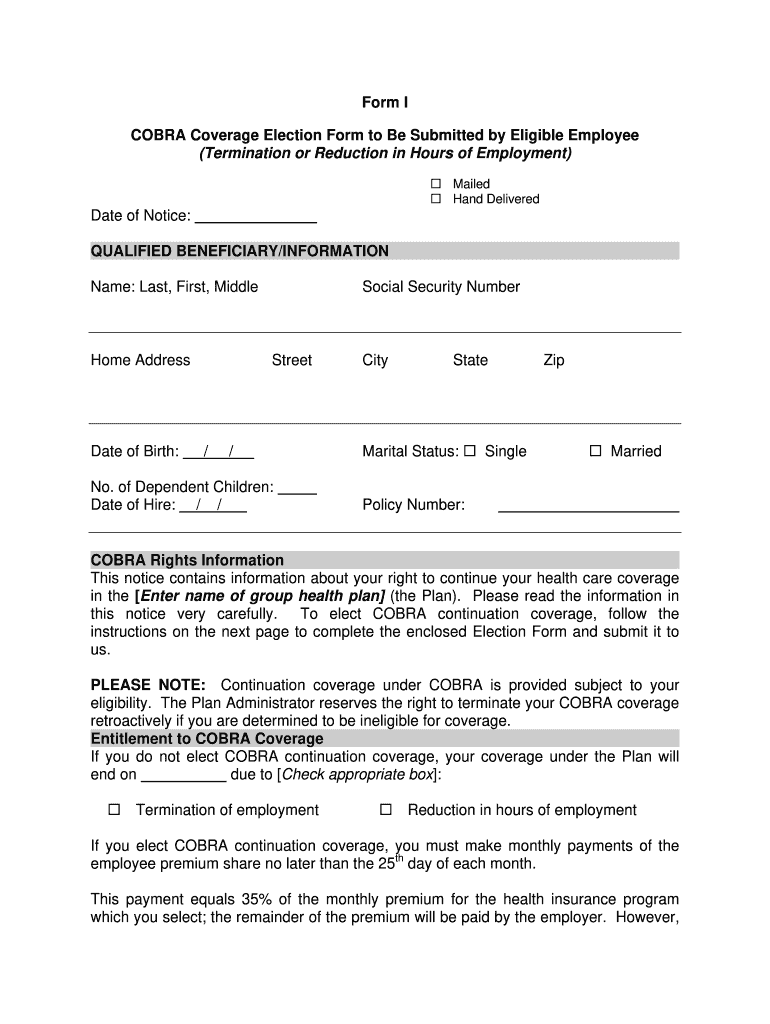
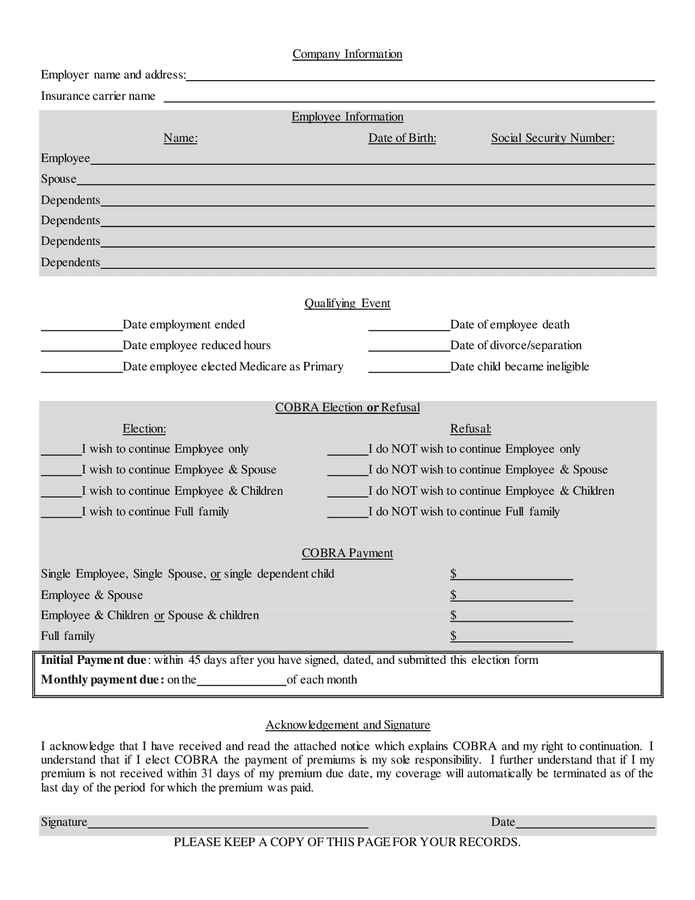
Cobra Form I Fill Online, Printable, Fillable, Blank pdfFiller
Plans must provide at least 45 days after the election (that is, the date the qualified. After the plan receives notice of a qualifying event, it must provide the qualified beneficiaries with an election notice within 14 days. Plans cannot require qualified beneficiaries to pay a premium when they make the cobra election. After receiving a notice of a qualifying.
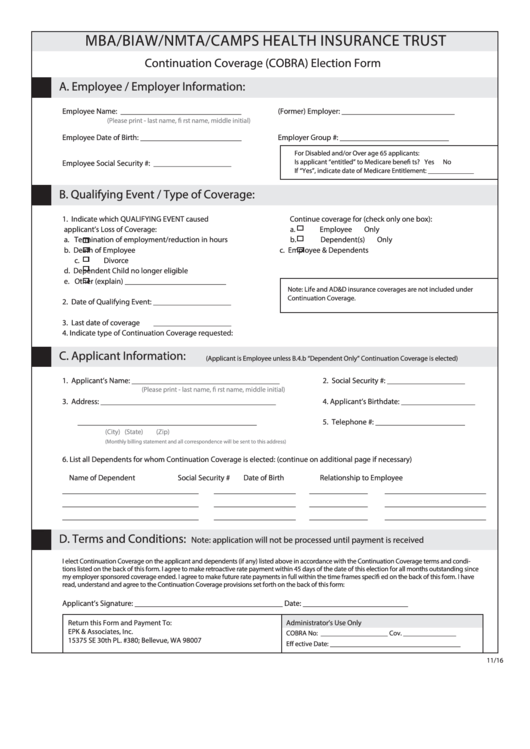
Top 9 Cobra Election Form Templates free to download in PDF format
After receiving a notice of a qualifying event, the plan must provide the qualified beneficiaries with an election notice within 14 days. After the plan receives notice of a qualifying event, it must provide the qualified beneficiaries with an election notice within 14 days. Plans cannot require qualified beneficiaries to pay a premium when they make the cobra election. Cobra.
CalCOBRA election form in Word and Pdf formats page 2 of 3
Plans must provide at least 45 days after the election (that is, the date the qualified. After the plan receives notice of a qualifying event, it must provide the qualified beneficiaries with an election notice within 14 days. Explore cobra continuation coverage options, eligibility, and benefits for workers, families, and advisers under hipaa regulations. Plans cannot require qualified beneficiaries to.
Continuation of Benefits Form Complete with ease airSlate SignNow
Cobra requires continuation coverage to be offered to covered employees, their spouses, former spouses, and dependent children when group health coverage would otherwise be lost. Explore cobra continuation coverage options, eligibility, and benefits for workers, families, and advisers under hipaa regulations. Plans cannot require qualified beneficiaries to pay a premium when they make the cobra election. Plans must provide at.
Cobra Form Net Template Fill Online, Printable, Fillable, Blank
Cobra requires continuation coverage to be offered to covered employees, their spouses, former spouses, and dependent children when group health coverage would otherwise be lost. Plans cannot require qualified beneficiaries to pay a premium when they make the cobra election. After receiving a notice of a qualifying event, the plan must provide the qualified beneficiaries with an election notice within.
COBRA election / refusal form in Word and Pdf formats page 2 of 2
After the plan receives notice of a qualifying event, it must provide the qualified beneficiaries with an election notice within 14 days. Plans cannot require qualified beneficiaries to pay a premium when they make the cobra election. After receiving a notice of a qualifying event, the plan must provide the qualified beneficiaries with an election notice within 14 days. Explore.
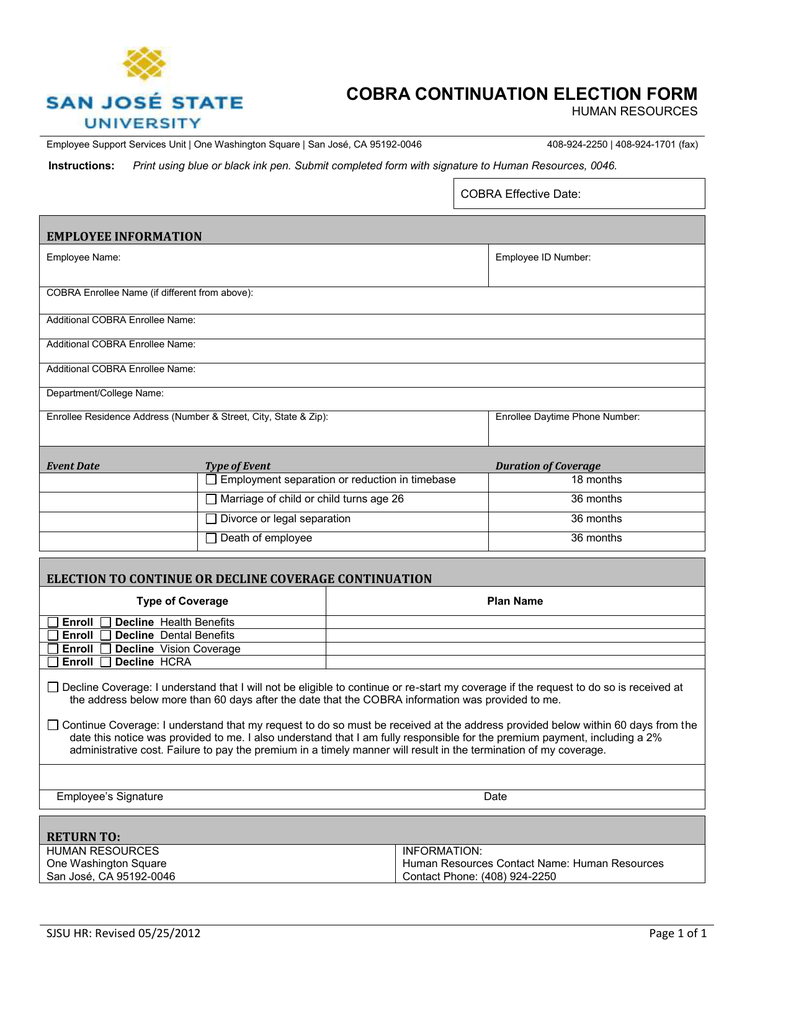
COBRA CONTINUATION ELECTION FORM HUMAN RESOURCES
Plans must provide at least 45 days after the election (that is, the date the qualified. Plans cannot require qualified beneficiaries to pay a premium when they make the cobra election. Explore cobra continuation coverage options, eligibility, and benefits for workers, families, and advisers under hipaa regulations. After receiving a notice of a qualifying event, the plan must provide the.
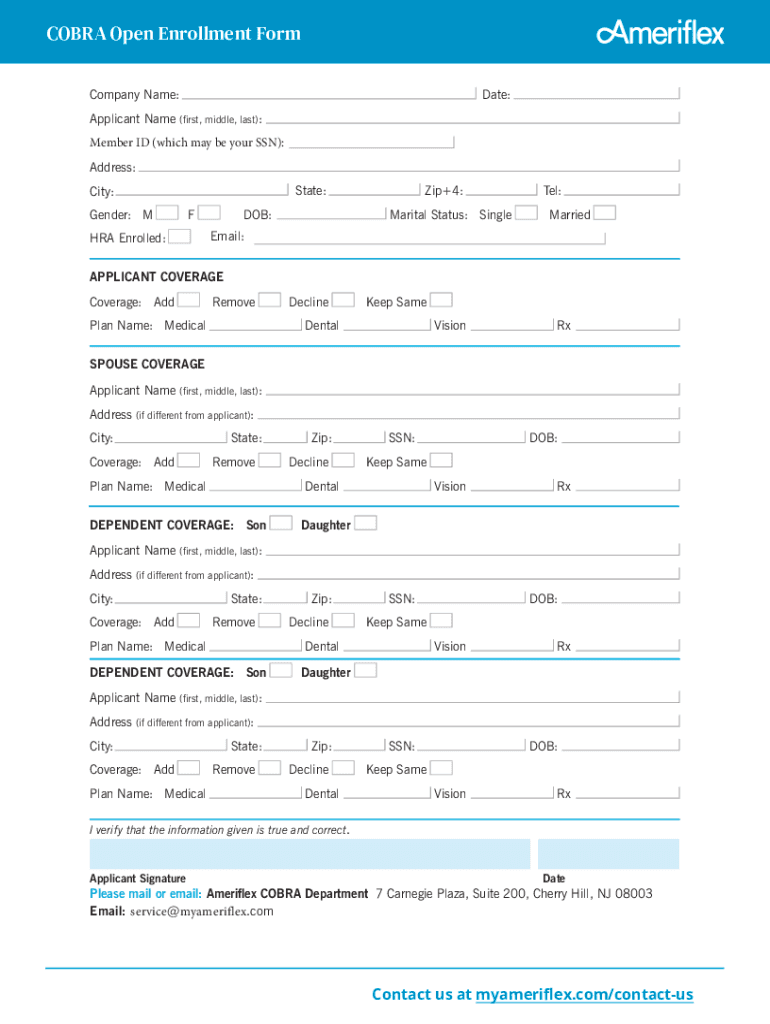
Cobra Open Enrollment Form Complete with ease airSlate SignNow
After the plan receives notice of a qualifying event, it must provide the qualified beneficiaries with an election notice within 14 days. After receiving a notice of a qualifying event, the plan must provide the qualified beneficiaries with an election notice within 14 days. Cobra requires continuation coverage to be offered to covered employees, their spouses, former spouses, and dependent.
Cobra Requires Continuation Coverage To Be Offered To Covered Employees, Their Spouses, Former Spouses, And Dependent Children When Group Health Coverage Would Otherwise Be Lost.
Explore cobra continuation coverage options, eligibility, and benefits for workers, families, and advisers under hipaa regulations. Plans cannot require qualified beneficiaries to pay a premium when they make the cobra election. After receiving a notice of a qualifying event, the plan must provide the qualified beneficiaries with an election notice within 14 days. Plans must provide at least 45 days after the election (that is, the date the qualified.